A pivotal debate is unfolding within the Advisory Committee on Immunization Practices (ACIP), the CDC’s expert panel, concerning the Hepatitis B vaccine. For over three decades, since 1991, this vaccine has been universally recommended for newborns – a practice now facing intense scrutiny and a potential shift in policy.
The current landscape mandates Hepatitis B vaccination for public school attendance in almost every state. However, a potential ACIP decision to limit the vaccine to infants born to mothers who test positive for the virus could dramatically alter these requirements, throwing decades of established policy into uncertainty.
Hepatitis B is a serious viral infection spread through blood and bodily fluids, typically contracted through sexual contact, shared needles, or during birth. While routine prenatal testing identifies mothers at risk of transmitting the virus to their babies – a scenario occurring in only about 0.5% of births – the universal vaccination policy has long been questioned.

The logic behind vaccinating newborns against a disease primarily contracted through adult behaviors has puzzled many parents. Why administer a vaccine for a sexually transmitted or bloodborne illness at the very beginning of life, before any risk exists?
Concerns regarding the safety of the Hepatitis B vaccine have been voiced by numerous medical professionals and parents alike, sparking a growing demand for a reevaluation of the current protocol.
During a recent ACIP meeting, Dr. Cynthia Nevison, a CDC contractor, presented a startling question: after 34 years of universal vaccination, has the program actually demonstrably reduced Hepatitis B cases across the population?
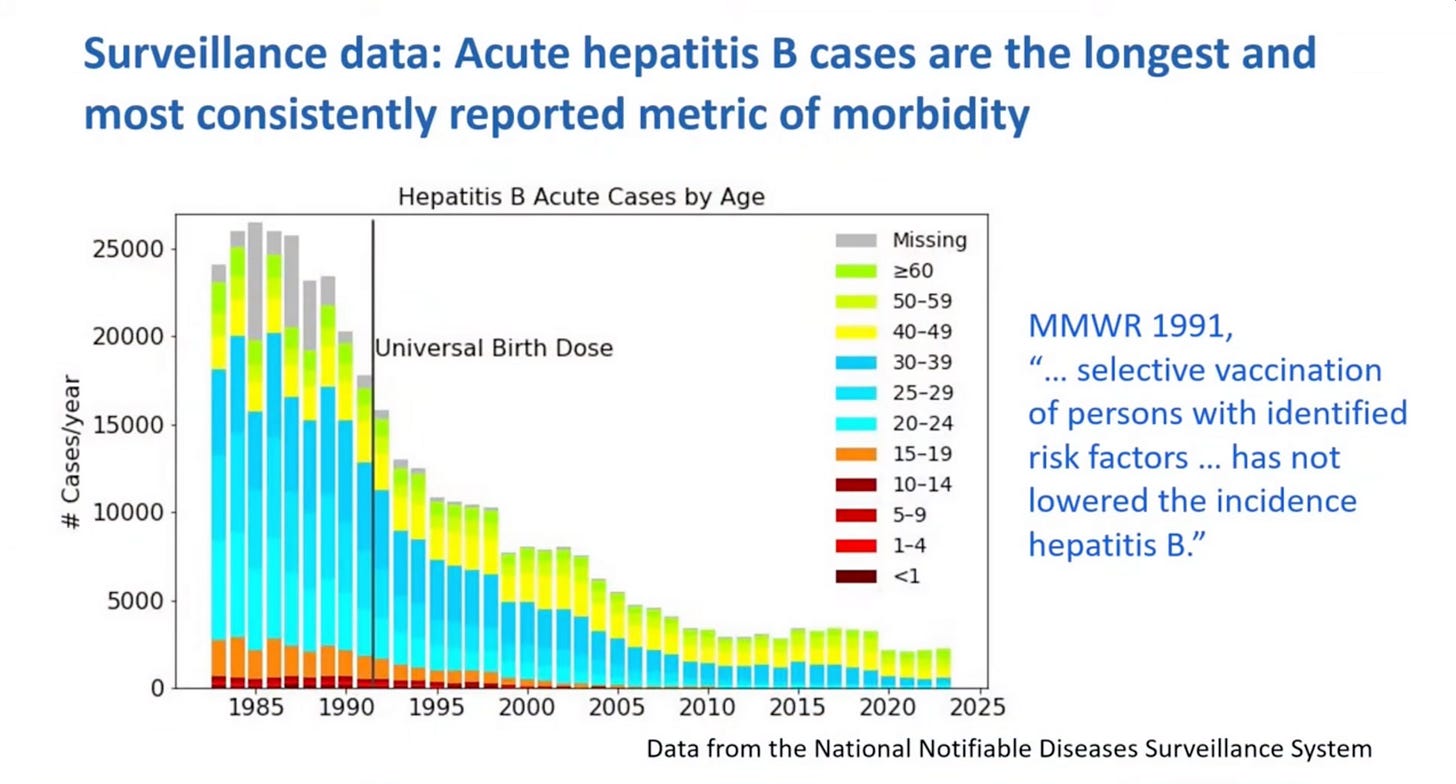
Dr. Nevison’s analysis of the data revealed a surprising truth. The decline in Hepatitis B cases began *before* the implementation of the universal birth-dose vaccination in 1991.
Examining trends across different age groups, Dr. Nevison pointed out that the reduction in acute Hepatitis B rates was already well underway in young adults – individuals who wouldn’t have been impacted by the vaccine for many years after its introduction.
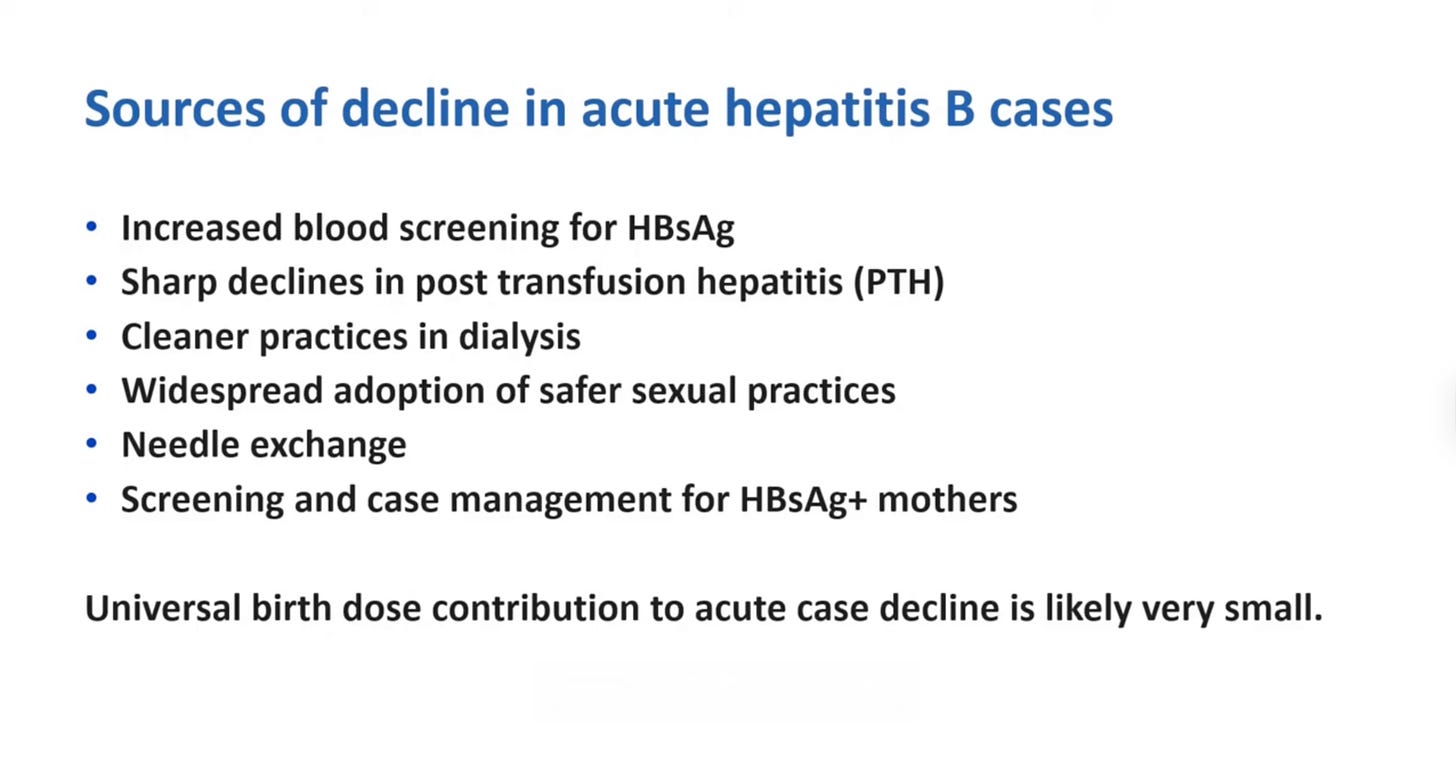
Her conclusion was direct: “universal birth dose contribution to acute [Hepatitis B] case decline is likely very small.” The vaccine, she argued, is not the primary driver behind the observed decrease in infections.
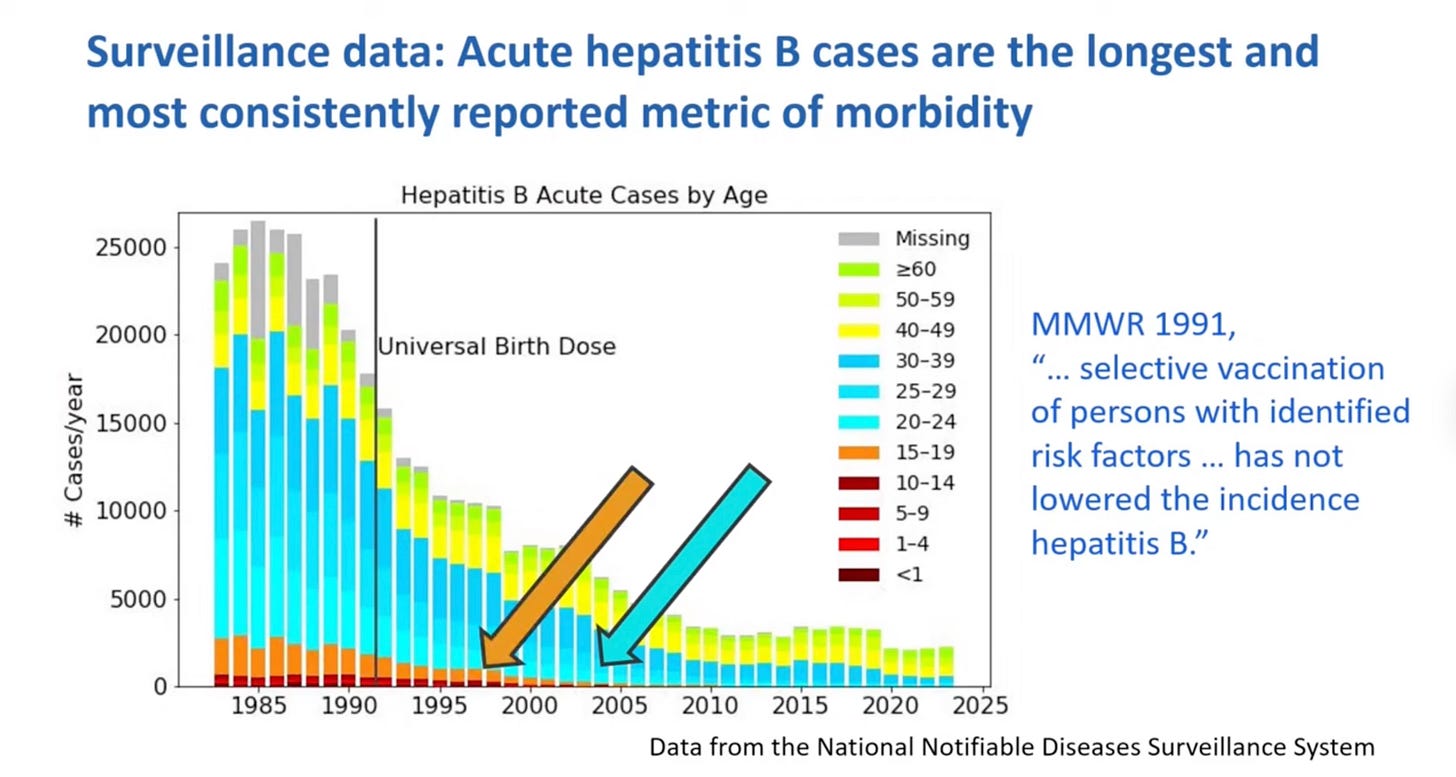
Instead, Dr. Nevison attributed the decline to several key factors: improved blood screening procedures, the adoption of safe sex practices during the AIDS epidemic, the implementation of needle-exchange programs, and targeted vaccination of infants born to infected mothers.
These measures, she explained, were already proving effective in curbing the spread of the virus both before and after the universal vaccination program began.
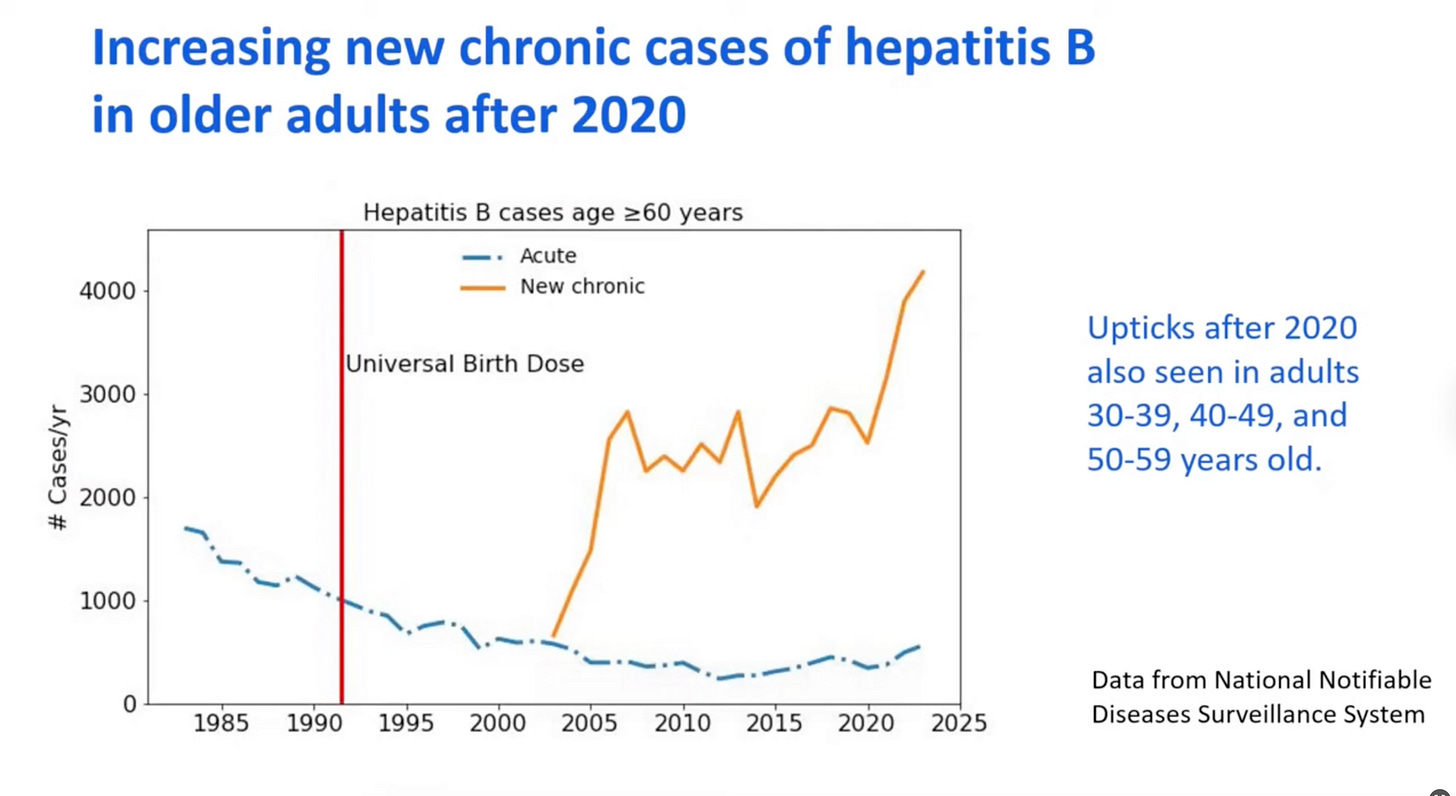
Adding to the concern, Dr. Nevison presented data showing a recent *increase* in new chronic Hepatitis B cases among individuals aged 60 and over since 2020. The cause remains unknown, but the universal birth-dose vaccine appears to offer no protection to this vulnerable population.
This revelation has fueled a growing movement to question the necessity of administering the Hepatitis B vaccine to all newborns. With only a small percentage of infants at risk of maternal transmission – and a high rate of maternal screening already in place – focusing on targeted vaccination makes far more logical sense.
Furthermore, the lack of a true placebo-controlled trial comparing long-term outcomes between vaccinated and unvaccinated children raises serious questions about the justification for universal administration.
Recent events, including concerns raised about the safety of other vaccines, may prompt a more cautious approach. The hope is that ACIP members will carefully consider the evidence and recognize the potential consequences of overconfidence in vaccination policies.